
Ultrasound Diagnosis of Medullary Sponge Kidneys
Share
Overview
Medullary Sponge Kidney (MSK), originally known as Lenarduzzi-Cacchi-Ricci disease, is a congenital disorder characterized by malformations of the terminal collecting ducts in the medullary region of the renal pyramids.
Dilation of these collecting ducts can cause medullary cysts of varying sizes (microscopically), which are often diffuse but do not involve the cortex.MSK is the definitive cause of renal calcinosis and renal calcium stones, but the clinical phenotype of MSK is more complex.
Etiology
1. Etiology
The disease is thought to be a congenital condition. The exact cause of MSK is unknown, though it is considered a congenital malformation. Infection and obstruction are considered secondary contributors. Many scholars view the disease as a congenital malformation of the renal medulla.
2. Pathogenesis
- In uncomplicated cases, the kidney is usually grossly normal or moderately enlarged. The lesion is confined to the cones and the cortex is not invaded.
- The pathology is characterized by dilation of the distal collecting ducts, leading to the formation of small cystic cavities lined with a single layer of epithelial cells. These cavities may contain mucous clots, calcifications, and small stones. The dilated collecting ducts communicate with the proximal normal collecting ducts, and the diameter of the junction with the calyces is normal or relatively reduced.
- The stones are often pure apatite or also contain calcium oxalate.
- The rest of the kidney is structurally and developmentally normal, but there is often chronic inflammation in the adjacent diseased renal tissue.
Clinical manifestations
More than 70% of MSK patients present with renal stones, typically located in the renal pyramids and mostly less than 1 cm in size.Many patients are asymptomatic early on, but symptoms may develop later, particularly if stones or infections occur.
The main symptoms include:
1. renal colic
2. hematuria and frequent urination
3. generally do not cause renal impairment, but a small number of patients due to the long history of the disease, repeated stone obstruction and infection, may produce secondary renal tubular acidosis, and later chronic renal insufficiency.
Imaging performance
1. Urography
The renal contour is smooth, and the renal shadow may appear normal or slightly enlarged. Multiple small stones (<10 mm) are often seen in the medullary pyramids, arranged in clusters, radials, or corn-grain patterns. Some stones may migrate into the calyces and become free stones.
2. Venous pyelography
Early filling of the dilated renal collecting ducts is visualized before the calyces. The pyramids show radiating coarse streaks of contrast-filled shadows. Multiple small, filled, spindle-shaped cystic shadows around the renal cones and calyces show bushy, bunch-of-grapes-like, or bouquet-like changes. The renal calyces are enlarged with protruding cups. After decompression, when the contrast agent in the renal pelvis and calyces has been emptied, the shadow can still be visualized in the dilated collecting duct for a period of time (forming the illusion of stone enlargement).
3. CT manifestations
- Scanning: CT scan shows dilated collecting ducts with small low-density cystic areas and multiple speckled stone shadows. These are clustered along the renal pyramids. The medulla is often enlarged, with associated thinning of the renal cortex and narrowing of the renal columns. - Enhancement: dilated renal collecting ducts early contrast filling and emptying more delayed renal cone can be seen in streaks or small capsular contrast aggregates stone shadow enlargement of the artifacts - excretion phase collecting ducts are filled with contrast, stones are masked by the filled contrast.
Ultrasound images
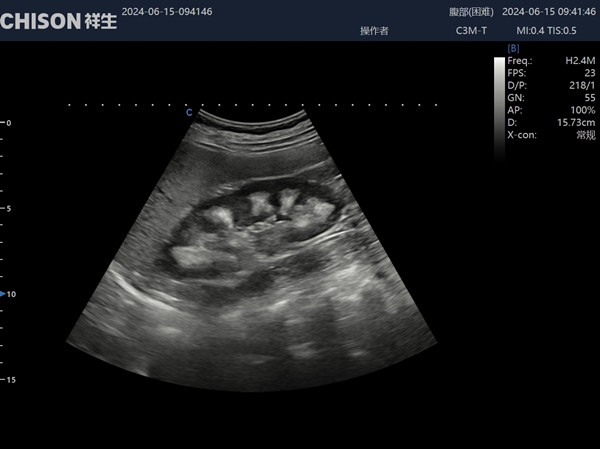
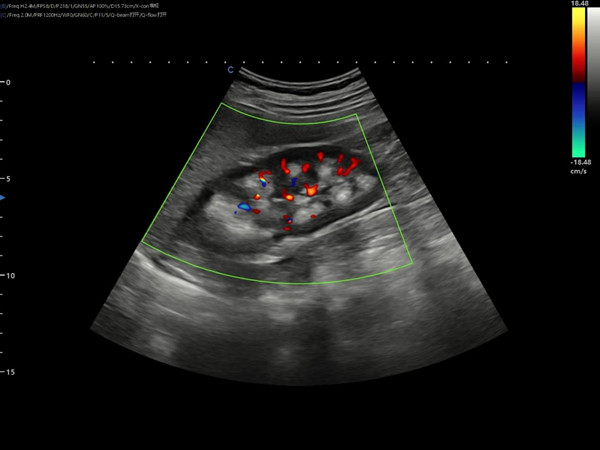

1. Renal cone echogenic enhancement: a strongly echogenic area with clear borders and radial rows.
2. Cone cystic structures: multiple anechoic areas of varying sizes are seen, mostly located in the papillary part of the cone.
Differential diagnosis
1. Renal calcinosis
- This condition is rare and is caused by pathologic deposition of calcium in the renal parenchyma.
- Calcification in and around the renal collecting ducts is more diffuse and typically involves both the renal cortex and medulla.
- There is no cystic dilatation of the collecting ducts or papillary cystic cavity formation.
- Often due to systemic, systemic diseases such as hyperparathyroidism (40%), renal tubular acidosis (20%) hypervitaminosis D, other pathologic hypercalcemia or hyperstatus.
- It is often accompanied by renal impairment.
2. Renal tuberculosis
- Most of the cases are unilateral, and the lesions are extensive and not limited to the medulla.
- Early stage of worm-like changes, with the progress of the disease may appear cavity and concomitant calcification (diffuse calcification, i.e., renal self-interception).
- The lesion may destroy the calyces and enter the renal hilum, thereby invading the ureter and bladder and leading to thickening of the renal hilum and ureteral wall (characteristic of tuberculous lesions).
- Laboratory tests, including urine culture and acid-fast staining, can help differentiate renal tuberculosis from MSK.
3. Gouty nephropathy
Gouty nephropathy, also known as chronic uric acid nephropathy, also shows hyperechoic renal parenchyma. Its ultrasound manifestations include blurring of renal periphery, shrinking of kidney, unclear demarcation of corticomedullary stroma, thinning of cortex, widening of medulla, and enhancement of medullary echogenicity, etc. Gouty nephropathy can be differentiated from MSK by correlating imaging findings with laboratory results and clinical signs of gout.
